With all the gluten-free food products flooding our supermarkets and bakeries and so many influencers and celebrities taking to Instagram to post their gluten-free recipes, one can’t help but wonder how everything sans gluten suddenly became the talk of the culinary world.
In the wake of this celebrity-endorsed gluten-free craze, it comes as no surprise that the UK’s gluten-free food market is expected to grow by GBP 203 million from 2023 to 2028 at a compound annual growth rate (CAGR) of 8.1% according to a report by Grand View Research.
While there’s no denying that more people are going gluten-free, it’s not just because of the latest diet trends. There’s good evidence that celiac disease is becoming more common. The results of a 2020 meta-analysis show that the incidence of celiac disease has gone up 7.5% every year in the past few decades in the Western world.
Today, celiac disease affects at least 1 in every 100 people in the UK. That’s roughly 683,500 people in total – a little over the entire population of Glasgow. The true incidence, however, may be a lot higher as only 36% of the people are clinically diagnosed.
While it’s not clear why more people are developing the disease, gastroenterologists believe that it is emblematic of a broader shift in global eating habits. We’re eating more refined wheat (especially in fast food) now than we ever did before, among other possible causes.
Is it affecting your body in more ways than you could imagine? You bet.
If you’re curious to understand how celiac disease can affect your oral health – yes, you read that right – stick around.
What is Celiac Disease?
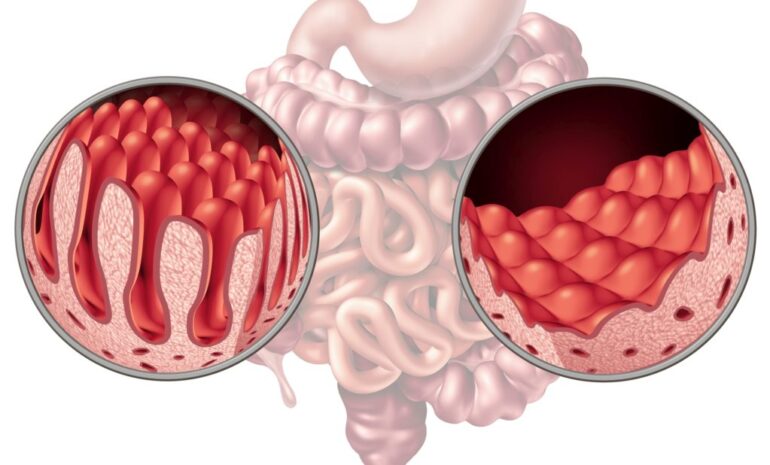
Celiac disease is a digestive disorder in which your immune system attacks and damages your small intestine when you eat anything that contains a protein called gluten. The autoimmune reaction destroys the villi, tiny finger-like projections lining the small intestine that absorb nutrients from the food into your body.
As a result, you’re unable to properly digest your food and get nourished by it.
The condition can remain silent for decades and then become apparent at any age.
Gluten is found in grains like wheat, rye, and barley, which are commonly used to make most pasta, cakes, breakfast cereals, and bread.
When anyone with celiac disease consumes gluten, it leads to a host of uncomfortable digestive troubles like bellyaches, nausea, bloating, constipation, and the like.
In the UK, half a million people remain undiagnosed. Those who are not avoiding gluten can risk developing serious health problems like iron deficiency anaemia, fertility issues, miscarriages, neurological problems, and even cancer. For women specifically, understanding how celiac disease may impact reproductive health can offer valuable fertility insights for women managing this condition.
Although it is mostly tummy troubles that your mind might instantly associate with celiac disease, there are currently 200 known signs and symptoms associated with celiac disease.
Among that constellation of symptoms are some distinct oral manifestations that are often overlooked.
Now, onto the burning question…
How Does Celiac Disease Affect Your Teeth?
Your body needs nutrients to function and perform various functions, one of which is the development of your teeth when you’re young.
Minerals like calcium and fluoride play a vital role in tooth development. Not absorbing enough from your food impairs the process and results in permanent structural damage.
Similarly, iron, vitamin B3, vitamin C, and folic acid are some other nutrients that keep your mouth healthy.
Nutritional deficiencies, along with immune disturbances, are the root cause of most of the oral effects of celiac disease.
Clinical Signs of Celiac Disease in the Mouth
The clinical signs of celiac disease can be different in children and adults and can be useful screening tools for your dentist.
Delayed tooth eruption and abnormal dental enamel
A delay in tooth eruption has been found to be the most common oral symptom associated with celiac disease, occurring in 47% of people with the disease, according to a PMC study.
Enamel defects are another common oral manifestation of celiac disease. A 2023 systematic review found enamel defects in 42% of people with the condition.
Children can develop celiac disease at any time, starting from when solid foods are introduced into their diet. If it happens before 7 years of age, while their permanent teeth are still developing, the process of enamel formation may be disrupted, and they might risk developing structural abnormalities in the dental enamel of their baby teeth.
The enamel may appear as patchy white-yellow tooth discolouration or have a rough surface with ridges, horizontal grooves, and shallow pits, giving it a mottled appearance. In severe cases, there could even be changes in the shape of teeth. These defects usually appear on the incisor and molar teeth.
As your enamel is the protective outermost layer of your tooth, damage to it could make your teeth weak and prone to decay and injury.
If the defects appear in baby or milk teeth, early diagnosis of celiac disease and adherence to a gluten-free diet can prevent them from developing in permanent teeth.
These defects are less common in adults.
What To Do
- See a dentist regularly
Regular dental visits can help spot these signs early, potentially leading to a quicker diagnosis and keeping the damage to a minimum. Additionally, maintaining oral health between visits can be supported with products like dental probiotics, available on Amazon.com.
- Get professional dental treatment
Although early diagnosis and treatment of celiac disease may help prevent future defects, it won’t, unfortunately, reverse those already present.
To fix those imperfections, you can get cosmetic dental treatments like veneers or composite bonding. Zental is an award-winning dental practice that offers exceptional cosmetic dental services. You can visit their website to book a consultation with a cosmetic dentist.
Dry mouth (Sjogren’s syndrome)
Having one autoimmune disorder can make you prone to getting another autoimmune disorder. 15% of people diagnosed with Sjogren’s syndrome, an autoimmune condition that causes dry eyes and mouth, have celiac disease, according to a Pubmed study.
With dry mouth, you have less saliva to naturally wash away food particles and debris and, therefore, are more susceptible to tooth decay and cavities.
What To Do
- Drink plenty of water to keep hydrated and get that saliva flowing.
- Try to cut down on alcohol, smoking, and caffeine, as they can dehydrate you.
- Chew sugar-free gum to boost saliva production.
- Your dentist may prescribe saliva substitutes to help keep your mouth wet and moist.
However, if you’re guzzling water like a camel but still battling a dry mouth, it’s possible that your gluten sensitivity might be the reason.
Mouth sores
Mouth sores are typical indicators of gut disorders, especially those that cause decreased absorption of nutrients. They can be present in both adults and children.
Also known as canker sores, these painful breakouts usually appear on the tongue or the inside of the cheeks or lips.
These painful sores can appear frequently due to nutrient deficiencies, particularly iron, folate, and vitamin B12 – all of which are common in undiagnosed coeliac patients.
What To Do
- Avoid eating acidic and spicy foods that could cause irritation.
- If the sores are too large or painful, see your dentist. They may prescribe you a topical anaesthetic or a mouth rinse to ease your symptoms.
If you have celiac disease, your ulcers will regress once you steer clear of gluten.
Other less common symptoms include:
Burning mouth syndrome
If your tongue feels like it’s been on the receiving end of a spicy food challenge (without actually eating anything spicy), it might be worth visiting a dentist and considering a gluten-free lifestyle.
Although not very common, experiencing a burning, tingling, or scalding sensation in the mouth can occur with no apparent cause. Known as burning mouth syndrome, it can happen as an oral side effect of celiac disease and usually resolves after sticking to a gluten-free diet.
A smooth tongue with loss of taste buds (atrophic glossitis)
In some instances of undiagnosed celiac disease, the tongue can be affected and experience soreness, a burning sensation, or inflammation.
A study in the New England Journal of Medicine suggests that these symptoms usually disappear within a month of avoiding gluten in the diet.
How can these clinical signs help you get diagnosed?
When your dentist notices any of the signs listed above, they might inquire about other symptoms and a family history of celiac disease.
If they suspect that you have celiac disease, they will refer you to a doctor to get it investigated.
Why is an early diagnosis so important?
When it comes to a condition like celiac disease, the sooner you get diagnosed, the sooner you can quit gluten and be on your path to recovery from the symptoms. It can also prevent serious complications from developing, both oral and general, of this disorder.
What Stands Out About Collaborative Care And Holistic Wellness?
The complex nature of the variety of symptoms linked to celiac disease is better tackled with a holistic, interdisciplinary approach that breaks down traditional medical silos.
Dentists can often be the first healthcare professionals to observe early oral manifestations, such as enamel defects, persistent mouth ulcers, and mucosal changes, that can be critical indicators of underlying gluten intolerance.
What do they do with these observations, you wonder?
Holistic dentists, such as those at Zental dental practice, focus on maintaining open communication and collaboration with gastroenterologists, primary care physicians, and nutritionists – basically, all those concerned with getting you well again.
The result? For you, this means timely referrals, targeted interventions, and a comprehensive treatment plan that addresses both oral and gastric manifestations of the disease.
With a more efficient diagnostic pathway, you won’t have to suffer unnecessarily long periods of pain and discomfort. No more running around seeing lots of doctors for various problems, all caused by one culprit: gluten. Or undergo serious damage to your oral and general health.
The long-term benefits? A collaborative approach means being provided with continuous monitoring of your progress, regular follow-up care, personalised nutritional guidance, and a holistic approach to managing the long-term health implications of celiac disease.
Just Your Oral Cavity, or Rather, A Mouthful of Clues?
If you or your kids often complain of stomach aches, determining whether your tummy trouble is run-of-the-mill or perhaps a more serious condition is not always simple. However, your dentist can play a significant role in diagnosing it.
You may now know this, but dentists are trained to note the signs and symptoms of this disease. A thorough medical, dental, and family history will usually be sufficient for them to suspect an underlying malady and point you in the right direction for further investigation.
If you’ve been experiencing any of the above-mentioned oral issues, your body might be hinting at an underlying gluten intolerance. Making that long-overdue trip to the dentist might, after all, prove to be more beneficial than you might realise.
Written by Hadia Hanif